Ask the Editor: Which Antipsychotic Is Best When Patients Complain of Akathisia?
The Carlat Psychiatry Report, Volume 16, Number 11 & 12, November 2018
https://www.thecarlatreport.com/newsletter-issue/tcprv16n11-12/
Issue Links: Learning Objectives | Editorial Information | PDF of Issue
Topics: Antipsychotics
Chris Aiken, MD
Dr. Aiken has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Each month, Editor-in-Chief Chris Aiken, MD, gives advice on a different practice challenge.
If you have a question you’d like Dr. Aiken to answer, please send an email to AskTheEditor@thecarlatreport.com.
Dr. Aiken won’t be able to answer all questions received, but he will pick one each month that is of general interest.
Which Antipsychotic Is Best When Patients Complain of Akathisia?
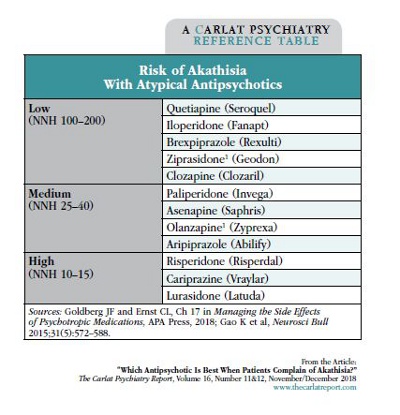
Akathisia is a sensation of inner restlessness so unpleasant that it independently elevates the risk of suicide. Among atypicals, quetiapine (Seroquel) has the lowest risk of akathisia, but that doesn’t mean it’s easy to take. Its other adverse effects, like sedation, weight gain, and hypotension, lead to more premature discontinuation and emergency room visits than with other antipsychotics (Hampton LM et al, JAMA Psych 2014;71:1006–1014; Zhou X et al, Int J Neuropsychopharmacol 2015;18:pyv060). So, it’s helpful to know the runner-ups. Rates are also low for iloperidone, brexpiprazole, clozapine, and possibly ziprasidone* and olanzapine*.
Newer is not always better. Cariprazine and lurasidone are among the worst offenders, but other new medications have lower rates of akathisia than the antipsychotics they were derived from (iloperidone and paliperidone < risperidone; brexpiprazole < aripiprazole). The highest rates are seen with high-potency conventional antipsychotics like haloperidol and fluphenazine.
The table lumps atypicals by their number needed to harm (NNH) for akathisia in schizophrenia. In mood disorders, the rates are higher but the pattern is similar. However, akathisia is difficult to measure reliably, and there are few head-to-head comparisons.
Akathisia is dose-dependent, so starting low and titrating slowly can help. Antidotes are numerous. Beta-blockers are first-line (propranolol 30–90 mg/day, betaxolol 10–20 mg/day). Treatments for restless leg syndrome can be helpful (rotigotine 2–8 mg/day, clonazepam 0.5–2.5 mg/day, gabapentin 300–1200 mg/day, amantadine 100–200 mg bid), and small studies support the use of 5-HT2A antagonists (trazodone 50–100 mg/night, mirtazapine ≤ 15 mg/night, cyproheptadine 16 mg/night) and vitamin B6 (600 mg bid).
*Studies are inconsistent, reporting both high and low rates.