The “Z-Drugs”: Safety Issues and Misuse Potential
The Carlat Addiction Treatment Report, Volume 8, Number 3&4, May 2020
https://www.thecarlatreport.com/newsletter-issue/catrv8n3-4/
Issue Links: Learning Objectives | Editorial Information | PDF of Issue
Topics: Anxiety | Clinical practice | Deprescribing | Free Articles | Pharmacology | polypharmacy | prescribing patterns | Risk Management | Sleep | Sleep Disorders
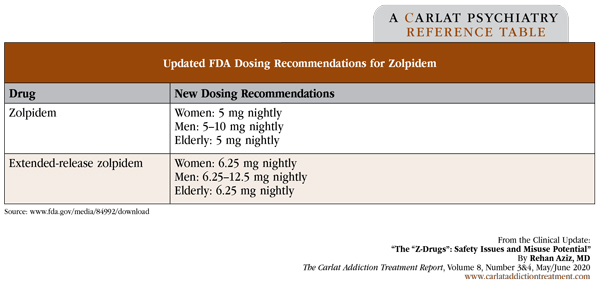
Rehan Aziz, MD. Associate Professor of Psychiatry and Neurology, Rutgers Robert Wood Johnson Medical School. Dr. Aziz has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity. Originally marketed as safer alternatives to benzodiazepines, the Z-drugs—eszopiclone (Lunesta), zaleplon (Sonata), and zolpidem (Ambien)—were considered devoid of misuse potential. But recent data and FDA warnings suggest we’ve been hitting the snooze on them for too long. Here, we review their risks and discuss safe prescribing. Medical risks Zolpidem has been associated with several side effects. From 2009 to 2011, it was implicated in 12% of all adult ED visits due to adverse drug events from psychiatric medications and in 21% of such visits involving adults 65 years or older. In both cases, this was significantly more than any other psychiatric medication. Adverse events included falls, head injuries, sedation, vertigo, and confusion (Hampton LM et al, JAMA Psychiatry 2014;71(9):1006–1014). Falls are a major concern in older adults, and unfortunately, zolpidem significantly increases the odds of a fracture (Kang DY et al, J Prev Med Public Health 2012;45(4):219–226). Complex sleep behaviors Motor vehicle accidents Risk of addiction, withdrawal, and overdose While these risks appear to be shared by all Z-drugs, zolpidem appears to confer a greater risk of withdrawal than zopiclone or eszopiclone. More prolonged use of zolpidem is also associated with greater likelihood of withdrawal. Symptoms of Z-drug withdrawal include insomnia, anxiety, euphoria, irritability, tremor, restlessness, speech difficulties, abdominal pain, hypertension, seizures, and delirium (Schifano F et al, Int J Neuropsychopharmacol 2019;22(4):270–277). Z-drugs carry a risk of overdose. This may be greater with zolpidem and zopiclone than zaleplon (Schifano F et al, 2019). Overdose risk may be particularly high when Z-drugs are combined with opioids. The risk of an opioid overdose when Z-drugs are used with opioids seems to be about the same as when benzodiazepines are mixed with opioids. Overall, patients exposed to opioids, benzodiazepines, and non-benzodiazepine sedative-hypnotics at any point are 60% more likely to overdose than those only exposed to opioids (Cho J et al, J Gen Intern Med 2020;35:696–703). What can clinicians do? The FDA has updated the labeling for zolpidem to reduce the risk of next-morning impairment Table: Updated FDA Dosing Recommendations for Zolpidem CATR Verdict: Prescribe Z-drugs with caution, especially with patients who are older, have comorbid psychiatric illnesses, and/or have a history of substance use disorders. Educate patients about complex sleep-related behaviors and avoid using Z-drugs if they’ve experienced such behaviors in the past. If Z-drugs are prescribed, use them short-term or intermittently, and regularly evaluate their continued use.
Zolpidem is the most widely prescribed hypnotic in the US and was the fourth most frequently prescribed psychiatric drug in 2013 (Moore TJ and Mattison DR, JAMA Intern Med 2017;177(2):274–275). Although generally recommended for short-term use, a national study in 2018 demonstrated that greater than two-thirds of patients prescribed zolpidem took it for longer than 3 months (Moore TJ and Mattison DR, JAMA Intern Med 2018;178(9):1275–1277).
Z-drugs have been connected to complex sleep behaviors. Examples include sleepwalking, sleep driving, and even things like sleep cooking, sleep eating, or other unsafe actions. The FDA has received reports of people accidentally overdosing, falling, getting burned, shooting themselves, and wandering outside in cold weather. The absolute number of reported events is low, however. Between 1992 and 2019, there were 66 serious cases of complex sleep behaviors, 20 of which resulted in death; that said, the actual number of cases is likely higher as these figures only include cases voluntarily reported to the FDA as well as 4 published cases (www.fda.gov/consumers/consumer-updates/taking-z-drugs-insomnia-know-risks).
There is an increased risk of motor vehicle accidents in patients prescribed benzodiazepines and hypnotics. The FDA has noted that zolpidem blood levels above 50 ng/mL appear capable of impairing driving to a degree that increases accident risk. The FDA found that 15% of women and 3% of men had zolpidem concentrations exceeding 50 ng/mL 8 hours after taking 10 mg of zolpidem. An even higher percentage of men (25%) and women (33%) experienced potentially impairing morning zolpidem levels after using 12.5 mg of extended-release zolpidem products (www.fda.gov/media/84992/download). These findings led to changes in the labeling and dosing of zolpidem.
Benzodiazepines still carry a higher risk of misuse and withdrawal than the Z-drugs, though Z-drug use disorders have been reported. Risk factors for Z-drug addiction include a history of drug use disorders and/or psychiatric illness (Hajak G et al, Addiction 2003;90(10):1371–1378).
Clinicians can reduce adverse Z-drug events by limiting them to short-term use for insomnia, and only turning to Z-drugs after considering other treatments such as sleep hygiene education, stimulus control therapy, sleep restriction therapy, relaxation strategies, cognitive behavioral therapy for insomnia (CBT-I), and safer medication alternatives. If zolpidem is to be used, warn your patients about the risk of next-morning impairment for activities requiring alertness, like driving. Patients should also know that impairment can occur even if they feel fully awake. Tell patients to take their medication immediately before bed with at least 7–8 hours of planned sleeping time.