Prior Authorizations for Psychiatric Medications: A Primer for Frustrated Clinicians
The Carlat Psychiatry Report, Volume 20, Number 4, April 2022
https://www.thecarlatreport.com/newsletter-issue/tcprv20n4/
Issue Links: Learning Objectives | Editorial Information
Topics: Practice management | Practice Tools and Tips | Prescription costs
Chris Aiken, MD.
Editor-in-Chief of TCPR. Practicing psychiatrist, Winston-Salem, NC.
Tony Thrasher, DO, DFAPA.
President, American Association for Emergency Psychiatry (AAEP). Medical Director of Crisis Services, Milwaukee County Behavioral Health. Clinical Associate Professor, Medical College of Wisconsin, Milwaukee, WI.
The authors have disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Prior authorization (PA) requirements for medications are time-consuming and frustrating for both clinicians and patients. In this article, we’ll describe how they work, how they affect patient care, and how to most efficiently work around them.
The basics
PA requirements began in the 1980s as a measure to rein in high-cost procedures like hospitalizations. As the price of pharmaceuticals rose in the 1990s, PAs were expanded to curtail branded medications, and in recent years their reach has expanded further to moderately priced generics like clomipramine. Today, one in four medications have some PA limitations, an increase from one in 12 in 2007, and physicians spend an average of 15 hours per week seeking PAs for their patients.
It’s hard to argue that PAs are a good use of clinicians’ time, but insurers also have legitimate reasons to steward the use of healthcare resources. Some prescribers are outliers who preferentially choose newer, higher-cost drugs, and that type of prescribing correlates with exposure to samples, pharmaceutical reps, and ads. In fairness, clinicians who are already inclined to prescribe branded drugs might be more likely to see reps, but at least one randomized trial suggests actual causation behind that correlation (Adair RF and Holmgren LR, Am J Med 2005;118(8):881–884).
How PAs work
While every insurance company’s procedure is different, typically a patient will learn about the need for a PA from their pharmacist when they try to fill a prescription. You will then be contacted by the pharmacy, which prompts the tedious process of figuring out why the medication was denied and gathering the information that the company needs to authorize the drug. The most common reasons for denial in psychiatry are:
Use of a newer and more expensive agent when cheaper generics are available
- Prescription of an unusual dose of a medication that falls outside the company’s guidelines
- Prescribing a medication that appears to the company to be off-label because they don’t have a record of the patient’s diagnosis
- At the beginning of the year, insurance company formularies often change, and patients may switch insurance policies—leading to a flurry of PA requests in January and February.
Tips for dealing with PAs
Use the CoverMyMeds website
CoverMyMeds (www.covermymeds.com) is a free website that partners with insurers to help clinicians efficiently complete PA forms. Some pharmacists will initiate a PA on CoverMyMeds and send you a key code to complete it; if not, choose “New Request.” You will need a copy of the patient’s insurance card for their pharmacy benefits as well as their diagnosis, demographic information, and a list of past medication trials.
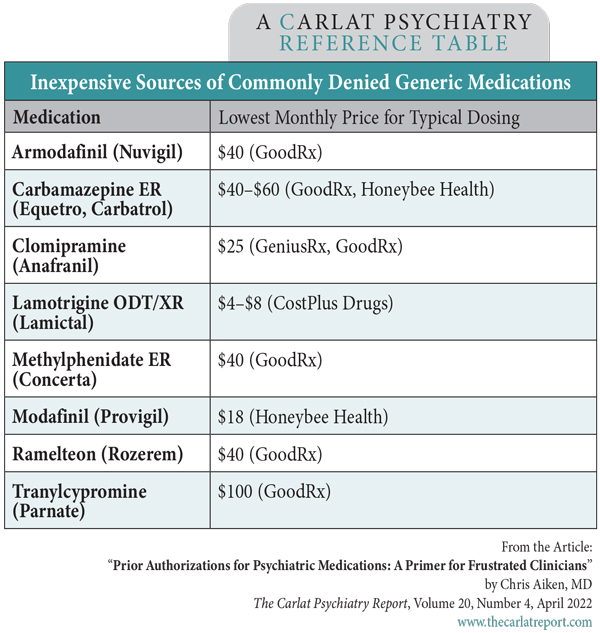
Table: Inexpensive Sources of Commonly Denied Generic Medications
Most PAs are approved within five business days, but delays of up to a month are not uncommon, particularly if the insurer requests more information. If the matter is urgent, you can usually request an expedited, 72-hour review, and plans purchased through the Affordable Care Act can grant a one-time fill while the decision is pending.
Appeal the stepped care requirement
If the diagnostic code matches the FDA indication and the patient has tried and failed generic options, the PA will usually succeed. If not, it can be appealed, but this process can take up to 90 days.
A common reason for denial is “stepped care,” where insurers require the patient to try cheaper alternatives first. Some states have outlawed stepped care, and other states limit this process when it creates unnecessary risks for the patient (for example, requiring a patient with diabetes to try olanzapine). If you practice in one of these states, mention the specific law and explain how it applies when requesting the PA (the National Psoriasis Foundation keeps an updated description of each state’s laws at www.steptherapy.com/step-therapy-legislation-by-state).
Other states have passed different types of laws easing the PA process. For example, starting in 2022, Texas physicians can bypass PAs altogether if they have a good track record of meeting insurance requirements in the past (specifically, they need a 90% success rate over six months to earn this “gold star” status).
If an appeal is unsuccessful, two federally funded programs might be able to support your case: the Office of Medicare Hearings and Appeals for Medicare plans, and the Consumer Assistance Program for other insurers. The process can sound daunting, but 75% of Medicare denials were ultimately overturned through appeal in 2017 (Resneck JS Jr, JAMA 2020;323(8):703–704).
Getting a better price
Rather than dealing with a PA, it might be quicker for your patient to find the medication elsewhere at a reasonable price, sometimes even less than their copay. There are several routes they can follow in their quest for cheaper meds.
Use low-cost pharmacies
Several new companies offer generic medications at low prices by negotiating directly with the manufacturer, such as www.honeybeehealth.com and www.geniusrx.com. Earlier this year, entrepreneur Mark Cuban joined the list with www.CostPlusDrugs.com. So far, Cuban’s drug store is the cheapest, with 18 psychotropics at around $5/month. The others have a broader selection, but CostPlusDrugs has an edge in one category: Half of its $5 offerings are for the modified-release formulations that are often not covered by insurance, including mirtazapine ODT, paroxetine CR, lamotrigine XR/ODT, and Depakote ER.
For patients who prefer to shop at a physical store, www.goodrx.com and www.rxsaver.com identify local pharmacies with the lowest cost on a given drug. Costco often rises to the top of these lists, and most states allow patients to fill prescriptions there even if they are not a Costco member. However, the lists often do not comprehensively index the online pharmacies, which can sometimes undercut even the cheapest brick-and-mortar price.
Tap into services for Indigent patients
Low-income patients who lack insurance may be eligible to receive both primary care and pharmacy services at a local free clinic (www.nafcclinics.org). The Patient Advocacy Foundation offers copay assistance to people who live in ZIP codes that have high levels of both poverty and medical morbidity (www.copays.org).
Most pharmaceutical companies provide branded medications at no cost to patients who qualify through their patient assistance programs. Clearinghouses like www.needymeds.org and www.rxassist.org can register your patients for these programs. To qualify, patients generally must have an income of $30,000–$48,000 (for individuals) or $40,000–$64,000 (for couples). Some programs consider the cost of the drug in determining those cutoffs.
Switch to a generic
When all else fails, you may have to switch to a generic. Fortunately, the list of brand-only psychotropics has shrunk to a handful of atypical antipsychotics (Caplyta, Fanapt, Latuda, Rexulti, and Vraylar), antidepressants (Emsam, Fetzima, Savella, Trintellix, and Viibryd), and hypnotics (Belsomra, Dayvigo), plus a longer list of stimulants. With stimulants, you can usually switch to a formulation that has the same ingredient but a different release mechanism, such as a generic version of Adderall XR, Concerta, Focalin XR, or Dexedrine Spansules.
Carlat Verdict:
Programs like CoverMyMeds ease PA requirements, but many patients can now get generic versions of commonly denied medications through discount pharmacies online.
For more on this topic, see Gold Star Program Reduces Prior-Auth Burdens.