Racism and Psychiatry
The Carlat Psychiatry Report, Volume 20, Number 5, May 2022
https://www.thecarlatreport.com/newsletter-issue/tcprv20n5/
Issue Links: Learning Objectives | Editorial Information | PDF of Issue
Topics: Black youth | Disparities | Diversity | Patient relationship | Race | Respectful Care
 Kali D. Cyrus, MD, MPH
Kali D. Cyrus, MD, MPH
Assistant professor, Department of Psychiatry, Johns Hopkins Medicine, Baltimore, MD. Physician-activist in private practice, Washington, DC.
Dr. Cyrus has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
TCPR: What does a psychiatrist need to know about race in this era?
Dr. Cyrus: Race and identity are hot topics, even for White people, so psychiatrists need to find a better way to talk about it. The pandemic brought the dynamics of oppression and inequality to the forefront in medicine. Racism is not just happening in the news, the protests, and the Black Lives Matter movement.
TCPR: Has psychiatry contributed to the history of racism in this country?
Dr. Cyrus: Psychiatry and medicine in general have not always been kind to people who are on the margins, people who are not White, people who are not cisgender, and people who are not able bodied or native English speakers. Historically, we’ve done things like experimenting on certain people who look a certain way or deliberately not explaining what we are doing or even telling them the opposite of what we are doing. For example, my patients comment often about being given a medication without much explanation, which leads to them not trusting the doctor or the psychiatric field. It helps to go the extra mile in explaining side effects, how the medication works, and the reason you’re recommending it.
TCPR: Some of these problems in psychiatry go way back, like drapetomania. Is that still relevant today?
Dr. Cyrus: Yes, it may be on the minds of some patients, either directly or indirectly. Drapetomania was a diagnosis applied to people who resisted slavery. It was referred to as a “mania for freedom” (Bailey ZD et al, N Engl J Med 2021;384(8):768–773). Samuel Cartwright invented the term in 1851. He also coined “dysaesthesia aethiopica” to explain enslaved people who had lost their motivation to work. Dr. Cartwright apprenticed under Benjamin Rush, whose image is on the seal of the American Psychiatric Association. It’s a reminder that we need to think about who created the standards for how we diagnose.
TCPR: What about involuntary hospitalization? Has that affected the Black community in certain ways?
Dr. Cyrus: That’s a good question, particularly today when so many states use the police to transport patients to psychiatric hospitals. We have a long history of overdiagnosing schizophrenia in Black males. We tend to go to the psychotic instead of the mood or bipolar category in that population (Gara MA et al, Psychiatr Serv 2019;70(2):130–134). Psychiatrists are also more likely to interpret Black patients as aggressive, and these biases have probably led to more involuntary hospitalizations in this group.
TCPR: How is this playing out in your practice?
Dr. Cyrus: Like with most mainstream events, I have seen external racial conflicts show up internally with my patients in both subtle and obvious ways. I had one patient who believed that President Trump sent the Secret Service after them because they were Black. Another feared going to the mall because there could be a shooter targeting Black people. Many of my current patients fear having to go back to the office to interact with their White colleagues. Much of their time in session is spent ruminating over distressing encounters involving White people. They present with insomnia, irritability, isolation, and apathy related to having to go to work, go to the grocery store, and generally interact with the larger world that puts them in a position to be discriminated against.
TCPR: Are more Black people seeking psychiatric help?
Dr. Cyrus: Since the pandemic, there’s been a surge in psychiatric visits in general. My experience is that Black people are included in this surge. They often tell me, “This is the first time I have seen a psychiatrist,” despite needing to see one for years. The pandemic’s events have made people more aware of problems that have simmered for decades. They see things on the news that have happened to them, their loved ones, or people who look like them. And watching harmful things happen makes people wonder whether trouble will knock on their door too—which has driven many to seek help (Brandow CL and Swarbrick M, Psychiatr Serv 2021 (Epub ahead of print)).
TCPR: They are seeing people who look like them get abused or killed by the police. What effect does that have?
Dr. Cyrus: When you start to see these images of Black people being killed, you worry that it will happen to you. And it’s not just the police. They are seeing incidents where armed citizens have gone out of their way to harm people out of some perceived fear—Trayvon Martin, Ahmaud Arbery, and the actions of Kyle Rittenhouse. At that point, the violence starts to feel more arbitrary, and you don’t know where it is coming from or if it could happen to you. For me, this means avoiding places that are mostly populated by White people or making sure I’m with someone who can be a witness if I do go to those places. Racism is not just a collection of negative experiences here and there. It can feel like an ever-present, bodily fear that you have no way to protect yourself from.
TCPR: Are some areas of the country more affected than others?
Dr. Cyrus: Racism and oppression happen everywhere—in liberal and conservative circles, in the South and California, and across health care settings. However, many people (myself included) use characteristics of an area to assess risk. For example, I live in DC, and if I am going on a road trip, I am much more careful and anxious while driving through states that have more conservative voting records, more flexible gun laws, and confederate flags hanging from the windows. While it’s statistically unlikely that something will happen to me because I am Black, I still have the stories of Ahmaud Arbery and Sandra Bland burned in my memory. The fear feels very real, and this reaction is very normal in the Black community.
TCPR: The divisiveness in society has raised the lid. Are you saying it has also made life feel less safe for non-White Americans?
Dr. Cyrus: Yes. It’s raised the lid without giving us the tools to repair. COVID-19 has added to the problem because we’ve been living apart under quarantine, and now we’re trying to figure out how to interact with each other again. Many Americans with oppressed identities don’t have a voice and are not in a position to explain everything. So what do they do? They talk with each other, and they talk on the internet.
TCPR: To talk, you need language. Can you bring us up to date on the new language that’s being used around these issues?
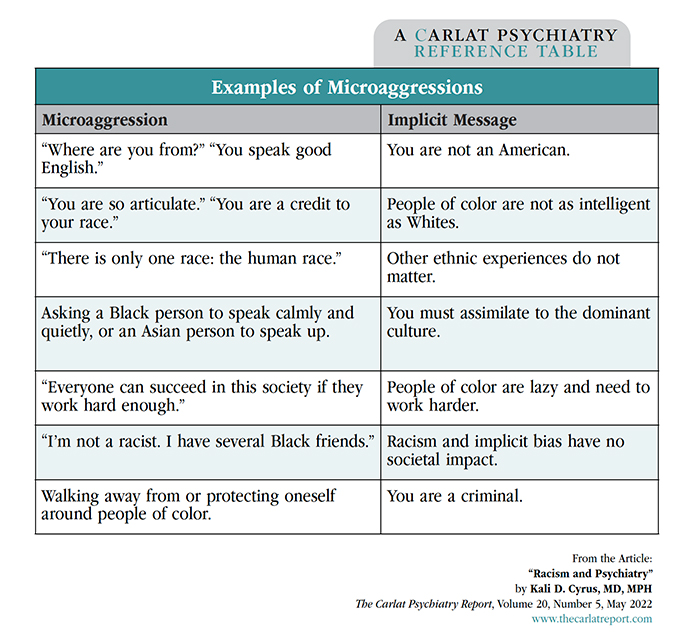
Dr. Cyrus: One term you’ll hear used a lot is implicit bias. This is when you can’t directly report how you feel about a certain group of people, but you have an unconscious preference for or against them. And when that bias is negative, it often feels to the victim like a microaggression, which is another term to know (FitzGerald C and Hurst S, BMC Med Ethics 2017;18(1):19). Microaggressions are everyday slights that may happen when you’re talking to another person, like misgendering them or calling them by a different name.
Table: Examples of Microaggressions
(Click to view as full-sized PDF.)
TCPR: Sounds like microaggressions are very common.
Dr. Cyrus: Yes. Most minorities have experienced them, but it doesn’t mean your patient will recognize them. To get by in society, they’ve had to brush them off and pretend they didn’t happen. Now that we’re talking more about racism and oppression, people who were once in denial about racist experiences are starting to recognize the impact those experiences have had on their lives. I also want to explain a bit more about racism, as there are a few more terms to know. Racism is discrimination that takes away resources from a group, based on race, that doesn’t have the same access to help as other groups. That discrimination can happen to other groups, like women, the differently abled, and Jewish people, and we call that sexism, ableism, or antisemitism. There are three levels of these “isms”: internalized, interpersonal, and systemic.
TCPR: Let’s go through those. What is internalized racism?
Dr. Cyrus: Internalized racism is insidious, and it shows up in practice. Essentially, it is accepting the negative messages you’ve heard about your identity. It’s almost like a self-hatred that can take varying levels of intensity, like feeling embarrassed, ashamed, or angry. People feel “lesser than,” especially in places where they are being evaluated, like on a date or at work. They don’t speak up because they fear being perceived as less intelligent. They overwork to compensate. It’s a mess of anxiety and unease, and many of my non-White clients have enjoyed working from home during quarantine just to get some space from all that. It may make people denigrate their own race and admire the other, as in the expression “the White man’s ice is cooler.”
TCPR: What is interpersonal racism?
Dr. Cyrus: Interpersonal racism involves the ways people interact, and it’s where microaggressions come in. Something offensive might be said to a person of color, or they may be ignored, passed over for promotions, or have their name constantly mispronounced. They may spend the whole day wondering, “Was that really directed toward me? Am I overreacting?” Neglect and omission are the interactions that particularly hurt.
TCPR: Are microaggressions different from trauma?
Dr. Cyrus: Microaggressions can be traumatic, but I think of them as little tiny cuts rather than a mortal wound like a trauma. It’s hard to say what’s “micro.” When I’m called “sir” in public (and I am a woman), is that micro to me? If I were a transgender woman and someone called me “sir,” how much would that hurt?
TCPR: Trauma involves a threat to life or bodily integrity, while microaggressions seem to reinforce a marginalized status.
Dr. Cyrus: Yes. Microaggressions often remind people of bad experiences they’ve had in a racist society, and for some those bad experiences include traumas the way they are defined in DSM-5. Psychiatrists like to categorize and delineate things, but how do you categorize the concept of spending your whole life in a racist society? Is that an ongoing trauma?
TCPR: Should we screen for microaggressions?
Dr. Cyrus: It’s a good idea. It conveys compassion. Ask, “Are there any social experiences that have been particularly traumatic and that you still think about?” “How have your identities impacted your experience?”
TCPR: How can we let the patient know we are on their side, even though we may blunder and fail to fully understand all they’ve been through?
Dr. Cyrus: Mistakes are inevitable. One strategy is to ask yourself, “What if I were someone from the opposite political party, someone from a different gender or race, or someone in a wheelchair?” Talk to people who are from different walks of life and learn from them. It’s not just the words we use, but everything down to how we design our office space. Are we making people who are different from us feel welcomed? Or are the magazines and decor in our waiting room the kind of stuff that would mainly appeal to psychiatrists?
TCPR: How can we make our offices more inclusive?
Dr. Cyrus: Patients who are used to interacting with people who don’t look like them are looking for clues that you’re safe. It helps to develop a mental routine where you walk into a room and think, “Whom is this space not amenable to?” Where is your office located? What are the houses like around you? Will people of a different gender or race feel safe there at night? What kind of magazines do you have? Do you have a rainbow flag anywhere?
TCPR: How can we open up that conversation in the consulting room?
Dr. Cyrus: Ask, “Are there differences between us that you are worried about—that might affect our interactions or my ability to understand and help you?” Even though there is a mismatch in the supply of providers who might look like some of these people of color, you have to be able to talk about race right now (Miu AS and Moore JR, Acad Psychiatry 2021;45(5):539–544). You are not going to be able to do it perfectly. The first step is just knowing that you’re going have to talk about it.
TCPR: Thank you for your time, Dr. Cyrus.