Telepsychiatry: What You Need to Know
The Carlat Psychiatry Report, Volume 13, Number 10, October 2015
https://www.thecarlatreport.com/newsletter-issue/tcprv13n10/
Issue Links: Learning Objectives | Editorial Information | PDF of Issue
Topics: Free Articles | Practice Tools and Tips
Daniel Carlat, MD Editor-in-Chief, Publisher, The Carlat Report. Dr. Carlat has disclosed that he has no relevant relationships or financial interests in any commercial company pertaining to this educational activity. The Carlat Psychiatry Report last covered telepsychiatry back in 2010. At that point, it seemed like a cool technology that some of you might want to use. Since then, telemedicine in general has taken off, with an estimated 67% of physicians using or planning to use telehealth in their practices. The appeal of telemedicine is clear, especially for psychiatrists. We are in great demand, and there aren’t enough of us to meet the demand—especially in rural counties. Since our diagnosis and treatment usually don’t require physical contact, we should be able to be quite effective via telepsychiatry. And patients are increasingly realizing that telehealth can save them the expense and time of schlepping to and from appointments. A recent study quantified the amount of time and money our patients waste by having to show up to appointments. Using surveys from the Bureau of Labor Statistics, the researchers found that the average amount of time patients spend per visit was 121 minutes (37 minutes in travel time and 84 minutes in clinic time—including both waiting for the doctor and time spent there). Using average wage estimates, this equated to an “opportunity” cost of $43/visit (Ray KN et al, Am J Manag Care 2015;21(8):567–574). So, the reasons to embrace telemedicine continue to mount, and luckily the technology has improved since our last article. Does telepsychiatry work as well as face to face? The most recent study randomly assigned 223 children with ADHD to 2 treatment groups. In the telepsychiatry group, children received 6 psychopharm visits by child psychiatrists delivered by videoconferencing. In the usual care control group, the children were treated in person by their PCPs who received telepsychiatry consultations. The kids in the telepsychiatry group did the best, significantly outperforming the PCP-treated group on all measures of ADHD (Myers K et al, J Am Acad Child Adolesc Psychiatry 2015;54(4):263–274). Among adults, one study of depression randomly assigned 167 Hispanic patients to either webcam treatment (6 monthly video sessions) or treatment as usual at a community health center. Webcam patients were more satisfied with their treatment and had a more rapid decrease in depression severity than TAU patients (Chong J and Moreno F, J E Health 2012;18(4):297–304). Who pays? A step-by-step guide Some of you may want to be more cautious, in which case there are many pay options out there. While we didn’t do a comprehensive survey, it appears that you can sign up for a HIPAA-compatible telepsych system for between $30–$300/month. This won’t break the bank, and they may have some advantages over Skype et al. The video quality will probably be better. Depending on the price, there will be added features, such as virtual waiting rooms, mobile access, automatic patient billing, and e-prescribing. Some reputable companies include Cloudvisit Telemedicine, evisit, Secure Telehealth.com, and Thera-link.com—listed in alphabetical order and with no implied endorsement. By the way, if you were to do a Web search on telepsychiatry companies, as we did, you may become confused. Most of the websites listed in the search results are actually staffing companies that sell telepsychiatric services to institutions such as community clinics, nursing homes, or prisons. You have to dig deeper into the sites to figure out whether they actually offer services to private practitioners. There’s a real Wild West feel to this industry, with many companies offering different services, making different HIPAA claims, and presenting bewildering pricing schemes that vary widely for offerings that are apparently equivalent. 2. Call your malpractice carrier. Most malpractice insurance policies will cover you for telepsychiatry, but you should check with your agent to be sure. 3. Check with your state medical board. In general, you must have a medical license in the state where your patient resides. A handful of states with dire shortages of physicians extend a special telemedicine license to out-of-state physicians. Some states require an initial in-person visit before you can practice telemedicine, but those are in the minority. Some state medical boards have very little to say about telemedicine. If that is the case in your area, you can follow the guidelines established by the Federation of State Medical Boards. 4. Inform your patients. Let your patients know that they have the option of seeing you via video visits, and have them read and sign a telepsychiatry consent form. Some examples of these types of forms can be found here or here. 5. Start seeing patients. Give your patients instructions on how to download whatever software you are using. Maintain professional standards as to your appearance (no pajamas!), and like any video encounter, be cognizant of what is in the background, noise level, etc. For 2013 practice guidelines on video-based tele-mental health services, see this page.
Before getting into the details of how to set up a telepsychiatry-capable practice, let’s look at the crucial issue of whether telepsychiatry even works. We now have several studies endorsing its efficacy.
Another study, which randomly assigned 126 women with PTSD to a trial of cognitive processing therapy either in person or via videoconferencing, found comparable outcomes in both groups (Morland LA et al, Depress Anxiety 2015 Aug 3 doi: 10.1002/da.22397).
Will insurance companies reimburse you for these visits? The answer is that it depends on the insurance. Medicaid is the most liberal, with 47 states allowing some reimbursement for telepsychiatry visits (see the website www.securetelehealth.com/index.php for great up-to-date information on various aspects of telepsychiatry, including insurance coverage). Medicare will reimburse for services if you are located in a designated underserved area of the country. In regard to private insurance, at least 30 states have passed laws requiring private insurers to reimburse telehealth to some extent. You’ll have to contact your patient’s insurance company to find out their policy.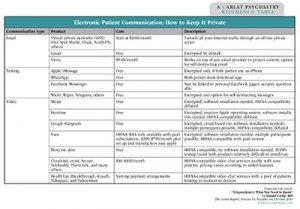
Table – Electronic Patient Communication: How to Keep It Private
Click to view full-size PDF.
1. Decide on your technology. Here you have two major choices: free and debatably HIPAA compatible vs. not free and pretty clearly HIPAA compatible. The major free services are Skype, Google Hangouts, and Apple’s FaceTime. In our article on HIPAA, we argue that the big three are “compatible enough” and that their convenience advantages outweigh the miniscule risks of a data breach. There are several other free or nearly free videoconferencing options now on the market that advertise themselves as being HIPAA compatible. We did some test runs of them (for more info, see our table, “Electronic Patient Communication: How to Keep It Private”).


