Treating Common Medical Conditions in Patients With Chronic Mental Illnesses
The Carlat Hospital Psychiatry Report, Volume 2, Number 5&6, July 2022
https://www.thecarlatreport.com/newsletter-issue/chprv2n5-6/
Issue Links: Learning Objectives | Editorial Information | PDF of Issue
Topics: contraception | Free Articles | hyperlipidemia | hypertension | hypothyroidism | medical conditions | Obesity | sexually transmitted diseases | urinary tract infections | UTI
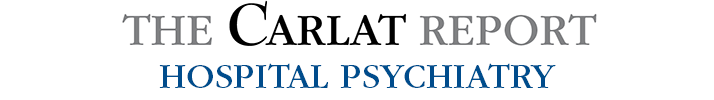
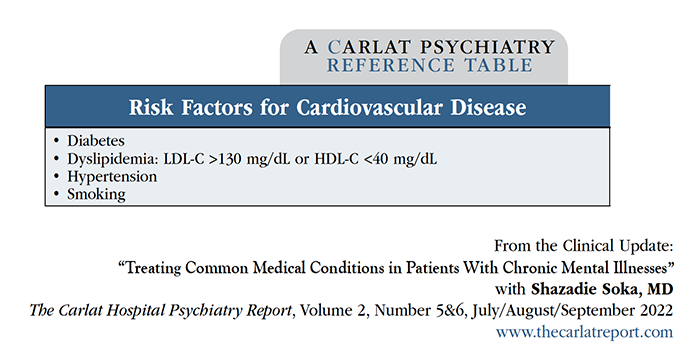
Shazadie Soka, MD. Chief resident, Wayne State University Department of Psychiatry, Detroit, MI. Lauren-Alyssa Wake, DO. Inpatient psychiatrist, Trinity Health, Minot, ND. Dr. Soka and Dr. Wake have disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity. After years of specialized training in psychopharmacology and psychotherapy, it can feel foreign or uncomfortable to prescribe a nonpsychiatric medication, such as an antibiotic, to a patient in need. Uncertainty about psychiatrists’ scope of practice leaves many of us feeling unsure about whether we should prescribe anything beyond psychiatric medications. Yet we also know patients with chronic mental illnesses frequently do not obtain treatment for common medical ailments, partly due to health care barriers as well as poor adherence with outpatient appointments. Our medical training should bolster our confidence that we can expand the narrow “scope” we’ve placed on ourselves. As medical providers, we want to diminish the barriers to health care and optimize our patients’ health outcomes. In this article we will review the treatment of common, uncomplicated medical conditions that we frequently encounter among our hospitalized patients with chronic mental illness: hypertension, hyperlipidemia, obesity, hypothyroidism, need for contraception, urinary tract infections (UTIs), and certain sexually transmitted diseases. Hypertension You probably don’t need to worry about isolated elevated blood pressure readings, but once you see a consistent pattern of elevated blood pressure across several encounters, it is reasonably likely that your patient has a diagnosis of essential hypertension. Make sure there are no concerns for hypertensive urgency or emergency (ie, SBP >180, DBP >120). Treatment options include an antihypertensive from the three main classes of drugs used for initial treatment—thiazide diuretics, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, and calcium channel blockers. Keep ethnicity in mind when treating hypertension: White patients typically respond well to lisinopril 10–40 mg daily, and Black patients do better with hydrochlorothiazide or chlorthalidone 12.5–25 mg daily. Thiazide diuretics can produce hypokalemia, so be sure to check and supplement potassium levels as necessary and avoid these medications in patients with sulfa drug allergies. Lisinopril is also a good choice for patients with diabetes. If your patient does not respond to these treatments, or if you have concerns for secondary hypertension or evidence of end-organ damage (ie, concern for chronic kidney disease or visual symptoms), refer to an internist. Hyperlipidemia People with chronic mental illnesses typically have one or more risk factors for cardiovascular disease, including elevated LDL-C levels. For which patients should we prescribe statins? The US Preventive Services Task Force recommends the use of statins for patients who meet all these criteria: Table: Risk Factors for Cardiovascular Disease Table: Statin Therapy How do you dose statins? Patients’ LDL-C levels guide the dosage or intensity of treatment (see table): High-intensity statins (eg, atorvastatin 40–80 mg daily) bring LDL-C levels down by 50% or more, moderate-intensity statins (eg, atorvastatin 10–20 mg daily) bring them down by 30%–49%, and low-intensity statins (eg, simvastatin 10 mg daily) bring them down by less than 30%. Don’t prescribe statins to patients with liver disease or who are pregnant or breastfeeding. Obesity We incorporate education about exercise and healthy diets in our patient encounters. For patients with antipsychotic-induced weight gain, we also prescribe metformin since it is more effective in treating antipsychotic-induced weight gain and increasing insulin sensitivity than exercise and diet alone (Wu RR et al, JAMA 2008;299(2):185–193). Metformin has minimal side effects and is safe to use, except for patients with renal dysfunction or metabolic acidosis. We initiate at 500 mg daily and titrate to 1000 mg twice daily. Table: Summary of Treatments for Common, Uncomplicated Conditions Orlistat is another medication to consider. Besides promoting weight loss, it decreases blood pressure, improves dyslipidemia, and decreases insulin resistance (Drew BS et al, Vasc Health Risk Manag 2007;3(6):817–821). Its main side effect is oily stool. We don’t prescribe this to pregnant women or patients with chronic malabsorption or cholestasis. Hypothyroidism Hypothyroidism is a relatively common chronic condition, and derangements in thyroid hormone may precipitate or exacerbate psychiatric symptoms. Psychiatrists have a long history of using thyroid medication to treat depression (Cooper-Kazaz R and Lerer B, Int J Neuropsychopharmacol 2008;11(5):685–699). The treatment of choice for hypothyroidism remains levothyroxine, a synthetic version of the thyroid hormone T4. The recommended starting dose for treating hypothyroidism is 100–125 mcg/day in otherwise healthy adults less than 50 years old and 25–50 mcg/day in adults age 50 or older. Increase by 12.5–25 mcg/day every four to six weeks until the patient becomes euthyroid. For patients with severe hypothyroidism, cardiac disease, myxedema coma, or stupor, seek consultation with an endocrinologist. Contraception Another need we frequently address is for contraceptive medications. Many of our female patients are at high risk for unintended pregnancies and have limited access to routine obstetrical and gynecological care. We include discussions on family planning in addition to prescribing contraception. Oral contraceptives remain the method of choice for most women (McCloskey LR et al, Am J Psychiatry 2021;178(3):247–255), but we’ve found that when we discuss the three-year duration of long-acting implantable contraception (eg, Nexplanon), many women opt for this instead. We reach out to our OB-GYN colleagues, who place the Nexplanon in a quick bedside procedure. Alternatively, we prescribe medroxyprogesterone acetate injection 150 mg IM, which is effective for three months. Hormonal contraception is safe, with some exceptions: We don’t use it for women older than 35 who are smokers, or women with histories of breast cancer, thrombotic disorders, liver impairment, or cerebrovascular disease. UTIs and sexually transmitted diseases You’ve probably seen many patients with sexually transmitted diseases, in part because psychiatrically unstable patients often display poor judgment and hypersexuality. Do you need to obtain a urinalysis if you suspect a UTI? Not necessarily—many primary care physicians treat suspected UTIs empirically, based on patients’ reports of dysuria, frequency, and urgency. Trimethoprim-sulfamethoxazole (TMP-SMX) remains the first-line treatment for uncomplicated cystitis, with a three-day course of medication carrying a bacterial eradication rate of 94% (Gupta K et al, Clin Infect Dis 2011;52(5):e103–e120). TMP-SMX is generally well tolerated but, like many antibiotics, can cause gastrointestinal side effects or rash. Dysuria, frequency, and urgency can also occur in urethritis due to gonorrhea or chlamydia, which can be easily checked with a urine test. We treat uncomplicated urogenital gonorrheal infections with a single 500 mg IM dose of ceftriaxone, and chlamydial infections with doxycycline 100 mg BID for seven days. CHPR VERDICT: By treating common, uncomplicated medical conditions, we can improve the health outcomes of patients who might otherwise not be able to access primary care. Hypertension, hyperlipidemia, obesity, hypothyroidism, need for contraception, STDs, and UTIs are readily treatable, with referral to a primary care physician for more complex cases.
(Click to view full-sized PDF.)
(Click to view full-sized PDF.)
(Click to view full-sized PDF.)